Frequently Asked Questions
According to the AOTA:
“Occupational therapy is the only profession that helps people across the lifespan to do the things they want and need to do through the therapeutic use of daily activities (occupations). Occupational therapy practitioners enable people of all ages to live life to its fullest by helping them promote health, and prevent—or live better with—injury, illness, or disability.”
If you think that sounds incredibly broad, you are correct! Occupational therapists work with all kinds of people in a wide range of settings and specialties.
People with chronic illness can have a wide range of things act as barriers preventing them from doing what they want and need to do. Sometimes those barriers are internal – such as pain or fatigue, sometimes they are from an unsupportive environment, and sometimes the barriers come from the activity itself. OTs can guide you through the process of addressing these barriers and utilizing the positive qualities of yourself, your environment, and your occupations to improve your quality of life.
Some concrete examples:
- OTs can help improve your access to quality healthcare through organization strategies, working on self advocacy skills, and providing recommendations for referrals to appropriate resources.
- Many people with chronic illness have disordered sensory processing. Sometimes it may feel like our senses are only there to overwhelm and frustrate us! OT’s can explore ways to cope when sensory input is overwhelming, prescribe exercises to improve sensory processing, and provide education on how you can use sensory input to your benefit.
- OTs can recommend and provide training for assistive technology at home, work, school, or out in the community.
- OTs can also recommend and provide training for strategies like energy conservation and joint protection that can help mitigate fatigue, pain, and risk of injury.
- Through comorbid neurodevelopmental conditions (Autism, ADHD, etc.) or symptoms like brain fog, some people with chronic illness may experience problems with executive function. OTs can work with clients to understand how executive dysfunction impacts them and to find effective strategies to stay organized, efficient, and productive.
- OTs work from a holistic point of view and can suggest changes to your social and physical environment to be more supportive of you and your goals. OTs can provide caregiver training, advocate on your behalf, and suggest adaptations that will make your physical environment more accessible. Many OTs in their spare time also advocate for the collective needs of their clients at the local, state, national, and international level.
There are even more ways people with chronic illness can benefit from OT, but hopefully this list gives you a basic idea of what OTs do.
Sensory processing (also often called sensory integration) is how you effectively take in, process, and use sensory information from your body and environment.
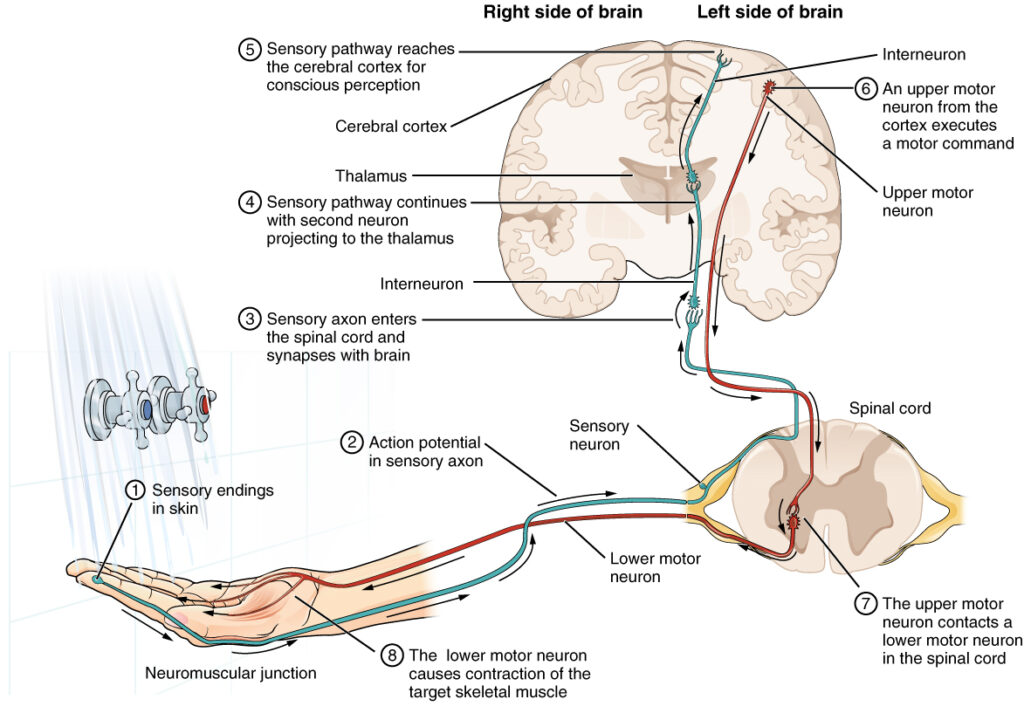
You can think of your sensory system as:
- The primary sensory organ – such as your taste buds.
- The nerves that take information from the sensory organ to the brain.
- The parts of the brain that process the sensory information.
- The nerves that leave the brain to communicate responses to the body.
- Your body’s response – such as spitting out something that is very bitter.
When something goes wrong in this path, your body may not react in expected ways to the environment.
You may have heard of Sensory Processing Disorder (SPD) which happens when one or more of your sensory systems have trouble handling sensory information to the extent that it causes symptoms and impairs function. SPD isn’t an official recognized diagnosis, but it is still a useful framework to describe and address sensory issues.
Though most commonly associated with Autism and ADHD, people with a range of health conditions can have trouble with their sensory systems and how they process sensory information. People who have Ehlers-Danlos Syndrome, brain injuries, multiple sclerosis, post-acute COVID-19, etc. can experience disordered sensory processing.
It depends who you ask! You probably grew up learning about The Five Senses – smell, touch, taste, hearing, and sight, but there are some scientists who would say that answer is 3, 8, or even over 20! It really depends on perspective and how human sensory systems are conceptualized. Occupational therapists generally organize your sensory experiences into 8 different systems.
| Sense | What is it? | What it is made up of? |
|---|---|---|
| Visual | Your sight – including the light, color, size, shape, and movement your eyes detect. | Visual receptors in your eyes, your brain, and the neurological paths to and from your brain |
| Auditory | Your hearing – including the volume, tempo, tone, and direction of sound. | Auditory receptors in your ears, your brain, and the neurological paths to and from your brain |
| Olfactory | Your sense of smell – (Did you know that smell is closely related to memory and taste?) | Olfactory receptors in your nose, your brain, and the neurological pathways to and from your brain |
| Gustatory | Your sense of taste. Sometimes OTs may include things like the texture of food or the coordination of your mouth, tongue and throat in this category. | The taste buds on your tongue, your brain, and the neurological pathways to and from your brain |
| Tactile | Your sense of touch including texture, surface pain, temperature, and vibration. | Several different types of receptors found in your skin, your brain, and the neurological pathways to and from your brain |
| Proprioception | Your sense of where your body is in space and how much force you are using. (People with hyper-mobility have impaired proprioception which can cause a lot of issues!) | Receptors in and around your joints, your brain, and the neurological pathways to and from your brain |
| Vestibular | Your sense of where your head is in space in relation to gravity and how your HEAD is moving – including acceleration/deceleration and direction | Receptors in your inner ear, your brain, and the neurological pathways to and from your brain |
| Interoception | Your sense of what is going on inside your body. Are you hungry or full? Does your tummy hurt? Do you have to go to the bathroom? | Chemical and mechanical receptors throughout your body, your brain, and the neurological pathways to and from your brain |
No one has perfect sensory processing and there is a lot of normal variation between people’s experiences. For example, you may like more spice in your food than your brother and he may like to listen to music at a louder volume than you do. You may get uncomfortable shivers at the feeling of a dentist drill and your best friend may not find the feeling uncomfortable at all.
Some people have differences that are great enough to cause a significant negative impact on daily function. It’s in these cases when someone might be considered to have sensory processing disorder or disordered sensory processing.*
Here’s what that may look like:
- Feeling spacey, anxious, or overwhelmed in crowds or busy environments
- Having poor posture or balance
- Clumsiness
- Feeling stressed or hesitant in unfamiliar environments
- Feeling reduced sense of safety even in safe environments
- Frequently having meltdowns, feeling overwhelmed, or “losing it”
- Feeling “burnt out,” tired or fatigued
- Tending to be active, boisterous, aggressive
- Needing physical activity throughout the day to stay alert and focused
- Having difficulty communicating ideas, emotions, or pain/discomfort
*Sometimes people who have issues in their primary sensory organ, (like the eyes in those with low vision or proprioceptive receptors in those with hypermobility) can have similar symptoms to those who have issues with sensory processing. Sometimes the same type of therapies we use with people with disordered sensory processing can improve symptoms.
Absolutely! Though some symptoms of disordered sensory processing can get better with age, many adults continue to struggle. Addressing the lack of resources for adults with disordered sensory processing is one of the main reasons why I started Empower OT!
First, we can define executive function as higher cognitive processes, or cognitive processes that regulate other cognitive processes. If your brain was a company, executive function would be upper management.
Executive dysfunction refers to when those cognitive processes aren’t doing their job. It can look like difficulty with planning, impulse control, emotional regulation, motivation, (cognitive) flexibility, organization, and self-assessment.
People can have executive dysfunction for a variety of reasons including damage to the frontal lobe, neurodevelopmental disorders (ADHD, Autism, etc.), mental health disorders, and dementia.
When someone has executive dysfunction, life can seem much more difficult than it is for others. People with executive dysfunction may have to spend a lot more energy to get the same work done, or aren’t able to do the work at all. They may have social difficulties, feel held back in their career, or “not live up to potential” in school.
Luckily, there are strategies that can address the negative impacts executive dysfunction has on your goals. OT can help!
In order to provide my clients with the best possible care, I have chosen not to accept insurance. Since you will be receiving treatment from an “Out-of-Network Provider” a Superbill will be provided at the end of each session that you can submit to your insurance provider for reimbursement. There is unfortunately no guarantee of reimbursement by your insurance company.
Initial Evaluation: a 60-90 minute comprehensive evaluation that includes medical and occupational history, goals, plan of care, and letter(s) to requested doctors or other health care providers. (A records release will be required due to HIPAA regulations.)
Cost: $300
Treatment Session: 45 min. of exclusive time with occupational therapist. May include additional “homework” or home program to promote formation and generalization of skills.
Cost: $125
Recommendations for School/Work Accommodations: a 1-2 page letter with specific recommendations and accommodations. This can include a phone consultation with involved parties. (A records release will be required due to HIPAA regulations.)
Cost: $125
Studies show telehealth can be a great option! Telehealth improves access to care, reduces delays in care, and promotes collaboration among your healthcare team. It has been shown to be effective in both pediatric and adult populations for a variety of specialized needs (source).
There are some situations when in-person services are needed due to equipment or hands on requirements. In those cases, recommendations for local clinics and programs can be provided to supplement or take the place of telehealth services.
Empower OT uses:
- Google Meet to host video calls
- Google Chat for messaging
- Gmail for e-mail
- Google Voice for phone calls and voice messages
- Ivy for payment
All of these are HIPAA compliant and chosen with your safety and security in mind.
In order to use these, you must have a computer, tablet, or smart phone with a working camera and any modern browser. You will also need a current email address and phone number. Payment must be done with a credit card.
To use Google Chat (optional) you will need to download the app or access it through a Google Chrome browser.
Otherwise, you do not have to download any apps or programs to communicate with me.